We apply various state-of-the-art techniques to study heart failure at several levels of (e.g. in vitro, in vivo, patient cohort studies, and clinical studies). We focus on developing representative in vitro models that can be employed to study molecular mechanisms of heart failure.
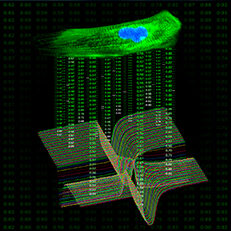
Gene discovery

We discovered several novel genes in the development and progression of heart failure. A common feature of the failing heart is the return to a pattern of fetal metabolism (concept of fetal reprogramming). With RNAseq we found that 5-oxoprolinase (OPLAH) was one of the most differentially expressed genes, unknown to play a role in the heart at that time.
Big data / biomarkers / AI
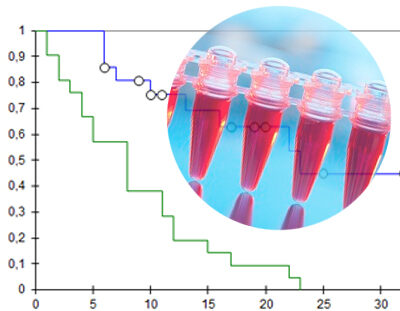
We use transcriptomics and proteomics to enhance our understanding of heart failure and apply AI to predict treatment response to guideline directed medical therapy.
3D tissue engineering / hiPSC
With the use human induced pluripotent stem cells in combination with advanced tissue engineering we developed a platform to improve maturation and contractility. These tools are used for disease modeling and validation of identified targets.
Peripartum cardiomyopathy

Peripartum cardiomyopathy (PPCM) is a rare but potentially fatal cardiac complication of pregnancy. The disease is characterized by heart failure in women presenting in the last trimester or in the first 5 months following childbirth. It affects between 1:1000-3000 pregnancies in Europe to 1:300 pregnancies in geographical hotspots like Haiti. Heart failure may spontaneously resolve in half of the PPCM patients; other patients may have persisting heart failure while up to 28% of patients die. PPCM is a complex disease and may be misdiagnosed due to clinical similarities with other pregnancy-related diseases (e.g., preeclampsia). Remarkably, PPCM can occur in women with an otherwise normal pregnancy. The cause remains unknown, but various risk factors have been proposed including age, ethnicity, nutrition, and number of previous pregnancies.
As part of a collaboration with the group of Denise Hilfiker-Kleiner, Martijn demonstrated that the 16 kDa prolactin fragment could only elicit a detrimental effect in the presence of plasminogen activator inhibitor-1 (PAI-1), which was previously unknown (Cardiovascular Research, 2020). In the search for the actual cause of the disease, Martijn generated induced pluripotent stem cell (iPSC) lines from multiple PPCM patients and healthy relatives. These iPSCs were differentiated toward cardiomyocytes that allowed him to study molecular pathways in PPCM patient-derived cardiomyocytes compared that could be offset to respective healthy cardiomyocytes. Through this comparison, it became clear that PPCM patient-derived cardiomyocytes could not effectively switch between different metabolic pathways when challenged (Circulation 2020).
PLN cardiomyopathy
Carriers of the PLN p.Arg14del pathogenic variant have a high risk of developing dilated cardiomyopathy (DCM) and/or arrhythmogenic cardiomyopathy (ACM) that may develop into heart failure. A founder mutation of this pathogenic variant was described by us and ±14% of Dutch DCM and ACM patients carry this pathogenic variant. Meanwhile, this pathogenic variant has also been found in other European countries, USA, Canada and in China, suggesting that it may be more widespread than originally anticipated. There is no established treatment for these patients other than standard heart failure therapy or heart transplantation.
We are the main PLN cardiomyopathy centrum in the Netherlands and together with our collaborators we investigate this syndrome at multiple levels in order to find therapeutic options to fight this disease. Amongst others, we participate in clinical PLN-R14del carrier registry, investigate clinical therapies (iPhorecast study) and investigate genetic and molecular aspects of this disease. The latter is performed in our own laboratory using state of the art techniques, including induced pluripotent stem cell (iPSC) technology, transgenic animal models and bioinformatics.
Micronutrients

Deficiencies in micronutrients, including iron and selenium, play a role in the pathophysiology of heart failure. In large cohorts we elucidated the relationship between these deficiencies and patient reported outcomes, including quality of life, exercise capacity and hospitalizations. Experimental in vitro models further helped us to elucidate the direct effects of these trace-elements on mitochondrial function.
Transthyretin amyloidosis cardiomyopathy
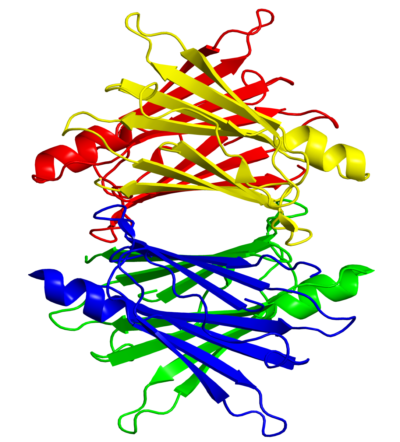
Transthyretin amyloidosis cardiomyopathy (ATTR-CM) is a specific form of heart failure characterized by the deposition of amyloid fibrils in the heart. ATTR-CM can be classified as sporadic, associated with the deposition of wild-type transthyretin (ATTRwt), or hereditary, associated with genetic variants of TTR (ATTRv). The prevalence of ATTR-CM is currently estimated at ~10% of patients with heart failure with preserved ejection fraction (HFpEF). Also in patients with severe aortic valve stenosis, ATTR is common. Diagnosis is however difficult and unfortunately often missed.
Until recently, ATTR-CM was considered an untreatable condition. However, several novel drugs are currently underway working on three levels: stabilizing TTR, inhibition production of TTR in the lever with RNA interference and removal of fibrils in the heart. For example a stabilizing drug (tafamidis), which is a small molecule that binds TTR in the plasma and promotes stability and a normal TTR conformation, was recently shown to improve survival and reduce hospitalisations in patients with ATTR-CM.
Amyloidosis research at the department of cardiology is highly interdisciplinary. Several studies are currently being initiated focusing on prevalence in the general HFpEF population and in patient with severe aortic valve stenosis. In this latter population direct hemodynamic effects of unloading are being investigated (AMYLO-TAVI). Together with the department of Nuclear Medicine and Internal medicine we participate in the I-CARE project. This project is a multinational consortium with partners in Germany and the UK and is financed by the Dutch Heart Foundation, British Heart Foundation and the DZHK. I-CARE will further shed light on the mechanism of action of stabilizing drugs and to identify responders versus non-responders.